Your cart is currently empty!
PAE FAQs
FAQs are developed in part through support from CDC and the Collaborative Initiative on Fetal Alcohol Spectrum Disorders (CIFASD).
What is prenatal alcohol exposure (PAE)?
Prenatal alcohol exposure occurs when an embryo or fetus is exposed to alcohol. Alcohol is a teratogen, a substance that during the nine months of gestation can cause malformations in human development.
How common is PAE? How many pregnancies in the U.S. are exposed to alcohol?
As reported in the January 7, 2022, edition of Morbidity and Mortality Weekly Report (MMWR), Centers for Disease Control and Prevention (CDC) researchers analyzed 2018–2020 data from the Behavioral Risk Factor Surveillance System (BRFSS) and found that nearly 1 in 7 pregnant people reported drinking alcohol and about 1 in 20 reported binge drinking in the past 30 days. In another study based on parental reports, nearly 26% of 9,719 adolescents participating in a U.S. National Institutes of Health study of brain development were prenatally exposed to alcohol (Association of Prenatal Alcohol Exposure With Psychological, Behavioral, and Neurodevelopmental Outcomes in Children From the Adolescent Brian Cognitive Development Study).
What factors contribute to the risk of PAE?
The primary factors that determine the risk of PAE are the quantity (the amount), frequency (how often), and the timing (when during a pregnancy) of the alcohol exposure. Children may be more affected by PAE if their mothers have poor nutrition or general health, smoke, consume marijuana, opioids, methamphetamine, or other illicit substances, live in environments where alcohol misuse is common and acceptable, experience adverse-living conditions or high levels of stress, or do not receive prenatal care. The genetic makeup of the mother or child and changes that turn genes on or off caused by alcohol exposure during gestation are believed to affect vulnerability to PAE, but have not yet been scientifically confirmed.
Are pregnancies exposed to alcohol also commonly exposed to other substances?
According to a 2020 article in Morbidity and Mortality Weekly Report, “The use of other substances was common among pregnant women who reported alcohol use—about 40% reported current use of one or more other substances.”
Is any amount of PAE or alcohol safe during pregnancy?
According to the published paper Drinking During Pregnancy and the Developing Brain: Is Any Amount Safe?, “The risks of light-to-moderate drinking during pregnancy are readily demonstrable in preclinical studies and some clinical studies. In contrast, the benefits of light-to-moderate drinking during pregnancy – the pleasure and relaxation afforded by alcohol – are modest. The current uncertainty over the effects of very low concentrations of alcohol on the developing fetus should be a source of reassurance for those women who have consumed a few drinks during pregnancy. At the same time, this uncertainty should be an impetus for women to refrain from any drinking while pregnant or trying to conceive.”
What is the current public health advice about PAE or alcohol during pregnancy?
Since 1981, the U.S. Surgeon General has advised that, “No amount of alcohol consumption can be considered safe during pregnancy.” Public health agencies, medical, behavior health, disability, and addiction associations, and research universities and institutes recommend complete avoidance of PAE. No published research has determined an amount of PAE that poses zero risk to an embryo or fetus or advises any amount of PAE that is known to be risk free.
What if I drank alcohol before I knew I was pregnant?
If you are pregnant and are drinking alcohol, the best advice is to stop drinking now and talk to your doctor about your alcohol use. The sooner you completely stop drinking the better it will be for your baby. Proper nutrition, good general health, a daily prenatal vitamin, avoidance of alcohol, tobacco, and other harmful prenatal exposures, and regular prenatal appointments all contribute to a healthy pregnancy.
What if I am finding it difficult to abstain from alcohol or I want more information about PAE?
Through FASD United, you can attend an online meeting of Recovering Mothers Anonymous, hosted by a nationally-recognized FASD expert, licensed addiction professional, and woman in long-term recovery. You can contact our Family Navigation Team at FASD United to be connected to a professional for a private conversation about PAE, or you can quickly find accredited alcohol treatment resources in the U.S. through the National Institute on Alcohol Abuse and Alcoholism (NIAAA) Alcohol Treatment Navigator.
Are postnatal nutritional supplements beneficial for children prenatally exposed to alcohol?
Initial scientific evaluation has found that children prenatally exposed to alcohol, “who received [the essential nutrient] choline had higher non-verbal intelligence, higher visual-spatial skill, higher working memory ability, better verbal memory, and fewer behavioral symptoms of attention deficit hyperactivity disorder than the placebo group. No differences were seen for verbal intelligence, visual memory, or other executive functions.” Four-year follow-up of a randomized controlled trial of choline for neurodevelopment in fetal alcohol spectrum disorder
Do genes play a role in the effects of PAE?
An abundance of evidence suggests genes do play a role in an individual’s susceptibility to FASD. While PAE causes FASD not every individual prenatally exposed to alcohol meets the criteria for FASD or exhibits any traits associated with the disorders, suggesting the existence of susceptibility or protective factors. The published research The Genetics of Fetal Alcohol Spectrum Disorders (FASD) explores the evidence for a genetic predisposition to FASD.
Is maternal alcohol consumption influenced by a pregnant woman’s partner?
Investigators found that “Partner influence is an important contributor to prenatal alcohol use,” and “Partner substance use and lower relationship satisfaction predict higher maternal alcohol use and depressive symptoms,” as reported in Partner influence as a factor in maternal alcohol consumption and depressive symptoms, and maternal effects on infant neurodevelopmental outcomes.
Can alcohol consumption by fathers before conception harm child development?
Animal studies have found that a father’s regular, significant preconception alcohol use can impact his offspring’s sensory perception, cognition, spatial reasoning, and language. If research determines paternal alcohol consumption before conception can permanently affect the development and behavior in a father’s offspring, those impairments would not be considered FASD. FASD occurs when an embryo or fetus is exposed to alcohol between conception and birth. The Impact of Paternal Alcohol Consumption on Offspring Brain and Behavioral Development.
Is adaptive function (daily living skills, socialization, communication) adversely affected by prenatal alcohol exposure?
“Although higher intellectual functioning was associated with better adaptive function ability among [non-alcohol exposed subjects], this was not found among the alcohol-exposed youth where a general dampening of adaptive ability was noted. Findings suggest that level of intellectual functioning of children with prenatal alcohol exposure does not fully account for caregiver-reported communication and overall adaptive function deficits,” as reported in Relation between adaptive function and IQ among youth with histories of heavy prenatal alcohol exposure.
Is there a correlation between PAE and preterm birth?
Research has identified an increased risk for premature birth associated with PAE and that preterm delivery contributes to the effects of PAE on development. See Gestational Age and Socioeconomic Status as Mediators for the Impact of Prenatal Alcohol Exposure on Development at Six Months.
Is there a correlation between PAE and sudden infant death syndrome?
Studies have found that PAE “Is a significant risk factor for SIDS and [other causes of] infant mortality [death during the first year of life].” Maternal alcohol use and sudden infant death syndrome and infant mortality excluding SIDS
Can prenatal ultrasound detect the physical features of FASD?
A study of 233 mothers and their children, Second Trimester Ultrasound as a Tool for Early Detection of Fetal Alcohol Spectrum Disorders (FASD), found that some ultrasound measurements were associated with selected facial features of FASD and lower neurobehavioral scores. However, the differences were relatively small, making ultrasound results alone an unreliable predictor of affected children.
Do birth mothers of children with FASD face discrimination?
FASD United Vice President and Spokesperson Kathy Mitchell and her coauthors report in The Public Stigma of Birth Mothers of Children with Fetal Alcohol Spectrum Disorders that “Research participants viewed mothers of children with FASD as more different, disdained, and responsible than women with serious MI [mental illness], SUD [substance use disorder], and jail experience.”
How can health care providers help reduce alcohol-exposed pregnancies?
“Health care providers can help to prevent alcohol-exposed pregnancies by providing their clients with factual information about alcohol and health and client-centered options for reducing their health risks,” as described in Applying Ethical Principles When Discussing Alcohol Use During Pregnancy.
Are there primary care practice guidelines for identifying and treating patients who are using alcohol or other substances?
The Centers for Disease Control and Prevention (CDC), an agency within the U.S. Department of Health and Human Services, has published, Planning and Implementing Screening and Brief Intervention for Risky Alcohol Use: A Step-by-Step Guide for Primary Care Practices. The guide describes a clinical preventive service that identifies and helps patients who may be drinking too much, only takes a few minutes, is inexpensive, and may be reimbursable.
Is PAE linked to congenital heart defects or disease?
Scientific findings in Prenatal alcohol exposure induced congenital heart diseases: From bench to bedside conclude that, “Prenatal alcohol exposure (PAE) is considered a key factor that leads to teratogenesis in CHD [congenital heart diseases] and its specific phenotypes, especially defects of the cardiac septa, cardiac valves, cardiac canals, and great arteries, adjacent to the chambers.” Early identification and drug supplements can help prevent PAE-induced heart disease.
Does prenatal alcohol exposure (PAE) have implications for adult physical and mental health?
The study, Prenatal alcohol exposure and health at midlife: Self-reported health outcomes in two cohorts, “evaluates self-reported health problems of midlife adults with and without a history of PAE.” Researchers from the Collaborative Initiative on Fetal Alcohol Spectrum Disorders (CIFASD) found that, “Compared with unexposed controls, individuals with PAE reported significantly higher frequencies of problems with hearing, dentition, heart, cancer, gastritis, kidney stones, bladder, diabetes, thyroid, skin, and seizures.” Findings suggest impairments associated with PAE persist into adulthood and amplify the importance of PAE prevention and early fetal alcohol spectrum disorders assessment and management practices.
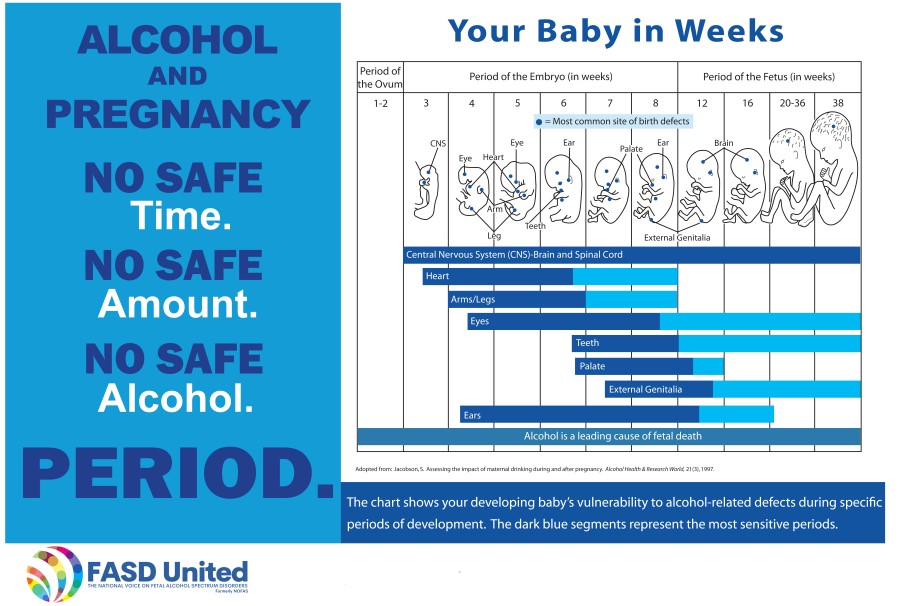
When during gestation is a developing baby vulnerable to PAE?
© FASD United, 2022, 2023, 2024
